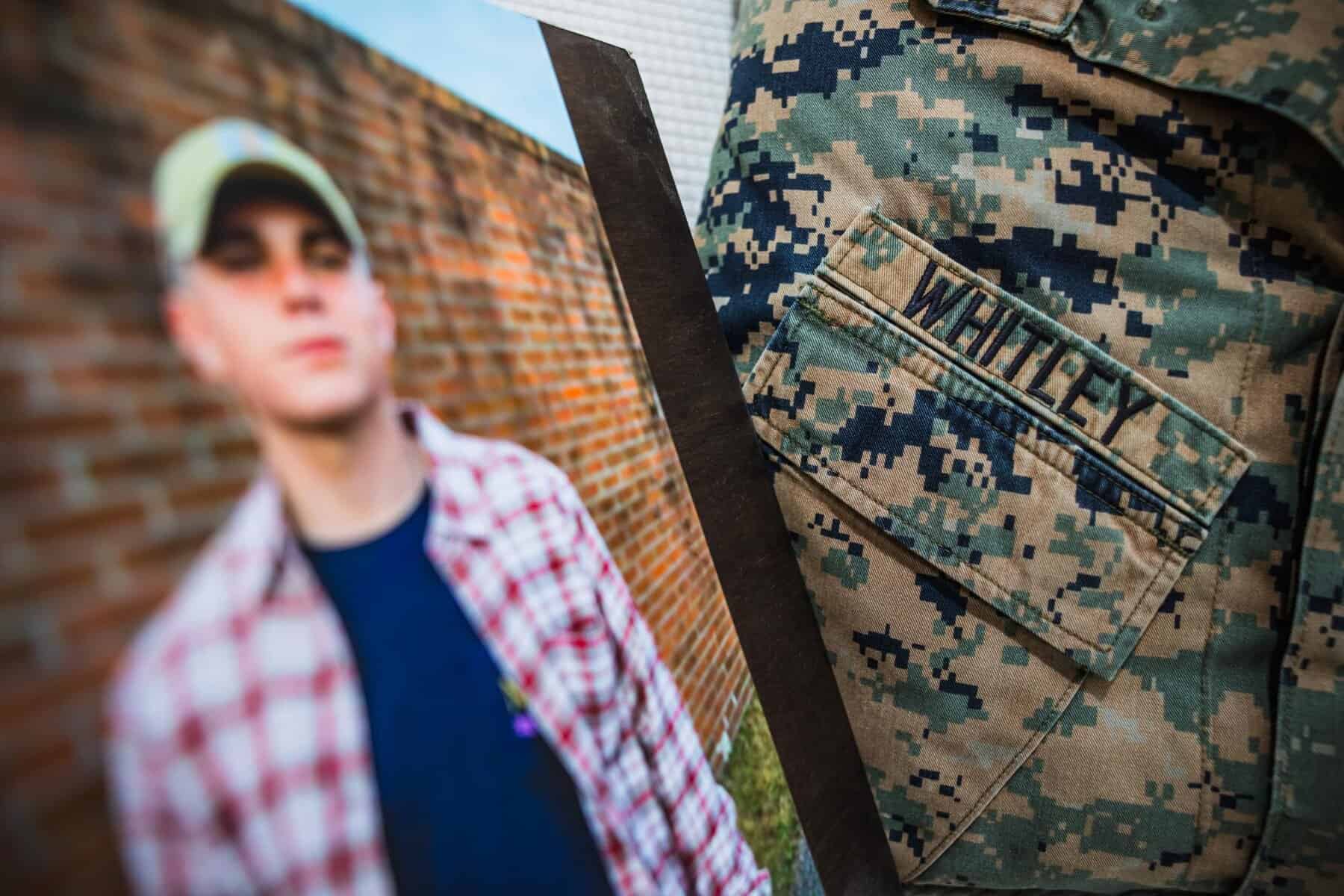
Hunter Whitley always wanted to be a Marine.
“That was his lifelong dream,” said Shannon McDaniel, Whitley’s mother. “We said, ‘Well, why the Marines?’ And he was like, ‘Well, they’re the badasses.’”
When Whitley graduated high school, he pursued his dream, going to boot camp in October 2018 and serving four years.
After Whitley was honorably discharged in July 2022, he returned to Alabama and sought outpatient mental health treatment from the Veterans Affairs Tuscaloosa Healthcare System while attending the University, receiving most of his treatment from the Tuscaloosa VA Medical Center.
Months later, in November 2022, Whitley — whom family described as a man with many passions, including music and art, and the type of person who cared about everyone — died by suicide. McDaniel wanted answers.
In September 2024, the VA Office of Inspector General, which provides independent oversight of VA, published a 53-page report detailing failures in Whitley’s treatment.
“I struggled for almost two years just trying to come to terms with Hunter wanted to die, and I need to be okay with it, because that’s what Hunter wanted, and Hunter usually got what Hunter wanted,” McDaniel said. But the OIG report, which came about after she filed a complaint, “changed everything.”
The report found that guidelines set by the Veterans Health Administration — the VA healthcare system — were not followed during Whitley’s treatment. According to the report, staff failed to do the following: adequately assess his suicide risk, address his reported access to a firearm, and provide appropriate education and oversight regarding potential adverse effects of an antidepressant he was prescribed, among other mistakes.
“This really is an example of almost every common error that’s made when somebody is at elevated risk for suicide,” said M. David Rudd, a professor of psychology at the University of Memphis and director of the Rudd Institute for Veteran and Military Suicide Prevention.

Veteran suicide is a national issue
According to a December 2024 VA report, in 2022, an average of 17.6 veterans died by suicide each day, and veterans were just over twice as likely to die by suicide as non-veterans. Suicide prevention is VA’s top clinical priority.
Veterans face many risk factors for suicide, experts say.
The transition from active duty to civilian life can be challenging, student veterans told The Crimson White.
Among other difficulties, such as income loss, the transition can cause veterans to lose their sense of identity and camaraderie, said Brianne Sampson, director of clinical support and emotional wellness for Hope for the Warriors, a national nonprofit that provides services to military families.
“When you’re a veteran, when that stability goes away, just disappears, it can feel very, very overwhelming,” said Blake Schickel, an Army veteran and current president of the UA Student Veterans Association, formerly known as the Campus Veterans Association. “You don’t have any of that structure anymore.”
Veterans also struggle with higher rates of substance abuse, traumatic brain injuries and PTSD than civilians, each of which is a risk factor for suicide. Several student veterans said they received traumatic brain injuries while in service.
At the Tuscaloosa VA system, Whitley screened positive for a TBI and was diagnosed with PTSD, the OIG report said.
His family members said his time serving during the withdrawal in Afghanistan in August 2021, in which American forces retreated while attempting to evacuate civilians, weighed on him.
However, Whitley’s family said he didn’t tell them specifics about what he witnessed during the withdrawal. The OIG report said that he reported in a substance use assessment completed at a military clinic having nightmares, flashbacks and anxiety since deploying, and denied suicidal ideation.

Like Whitley, Schickel served at the Hamid Karzai International Airport in Kabul that was at the heart of the civilian evacuation and was where a suicide bomber killed 13 American service members and over 160 civilians.
Schickel, who struggled with what he experienced, said he believes many service members obtained “moral injuries” from the deployment, especially as many civilians died. Discussing what they saw can be difficult, in part as some service members feel command could have executed the evacuation better to save more civilian and service member lives.
“Rehashing that deployment for most people leaves you feeling pretty upset, pretty angry,” he said.
Failure to address and evaluate suicide risk
According to the OIG report, medical professionals did not properly treat Whitley for a potential TBI nor assess and address his suicide risk, failing to work with him to restrict his access to firearms.
A nurse practitioner at a clinic did not follow up after he screened positive for a TBI, as they did not know it was their responsibility to do so.
In another instance, a different nurse practitioner at the VA medical center didn’t complete a required suicide risk screening at his mental health intake appointment, completing a briefer one used in the facility’s intake template.
Though Whitley denied thoughts of suicide, the report said his suicide risk might still have been inadequately assessed in the brief assessment. Again, the nurse practitioner denied knowing the screen was required.
Days before he died, in a depression rating scale, Whitley reported moderately severe depression symptoms, and thoughts of being “better off dead” and harming himself. The OIG said a social worker at the medical center who reviewed the rating scale should have sought further evaluation or supervision or consulted with Whitley’s prescriber, but didn’t.
Whitley also reported to the social worker that he had access to a firearm — another suicide risk factor — which according to the OIG and experts, should have warranted further analysis of his risk and discussion of safe storage practices; although, after he reported access to firearms, no lethal means safety counseling was conducted to restrict access to “lethal means” like firearms.
“If one of them, just one of them, had done one thing they were supposed to do, then he might still be here,” McDaniel said of the staff.
VA encourages providers to engage family members whenever possible in lethal means counseling, including by asking them to take temporary possession of firearms.
Experts say medical providers should include family in discussions about mitigating risk with firearms, but that doing so requires patient consent. McDaniel said the Tuscaloosa VA did not do so.
“It’s not required or mandated. This is common sense,” said Tamar Rodney, a mental health nurse practitioner and assistant professor at the Johns Hopkins School of Nursing.

The social worker cited Whitley’s reported lack of a suicide plan or a previous suicide attempt, and the presence of certain protective factors, such as Whitley’s positive future plans and support system, as reasons for not following up on his reported suicidal ideation.
The report noted that a supervisor failed to adequately oversee the social worker’s treatment, which could have contributed to the social worker’s inadequate assessment of suicide risk and lack of lethal means counseling.
A VA spokesperson and a spokesperson for the VA Tuscaloosa system acknowledged requests for comment for this story but did not provide comment in time for publication.
In a statement in November 2024, former VA Press Secretary Terrence Hayes told CBS 42 that the Tuscaloosa system was taking specific steps to address the report’s findings.
The system agreed to address all 14 recommendations made by the OIG, such as by tightening oversight of clinicians and creating new standards for patient care. Before the report released, the facility also made other changes, like adding the required suicide risk screening to mental health intake templates.
“Suicide prevention remains our top clinical priority, and we are committed to continuous improvement and accountability,” the statement said. “Our goal is to ensure that every Veteran receives compassionate, timely, and high-quality care.”
Deficiencies with required suicide screenings are a nationwide issue at Veterans Health Administration facilities, according to a separate OIG report published in December 2024.
Issues stemmed from a lack of training, oversight and accountability to enforce compliance. The report found that in settings like intake mental health appointments, where suicide screenings are required, the VHA did not monitor facilities’ adherence.
Lethal means training, execution and documentation was also a problem in VHA facilities, a November 2022 OIG report found. In 12 cases where patients had firearm-related suicides, providers had failed to document one of more of the following: required suicide evaluations, assessments of firearm access or safe storage discussions.
The VHA agreed to specific measures to address issues raised in both investigations, the reports said.
Similar stories
In several ways, Whitley’s story mirrors that of other veterans who died by suicide. Other parents who spoke with The CW said their sons, who also died by suicide, had TBIs. All three received psychotropic medications from the VA, and all three parents requested OIG investigations into their sons’ treatment.
Tracie Everett’s son, Benjimen Tyler, served seven years active duty in the Army before settling in Pueblo, Colorado. His mother, who lives in Georgia, described him as charismatic and loving. But like Whitley, Everett’s son suffered with his mental health after his discharge.
“The military took my son away,” she said, noting the transition to civilian life was difficult for her son. “I gave him to the military a happy, healthy, grounded, God-loving, caring person.” Years later, she “got a broken boy.”
Like Whitley, Tracie Everett’s son died using a firearm in May 2022.
According to an email sent by the OIG to Everett, the OIG opened a case for further review after staff reviewed a complaint she filed about her son’s outpatient mental health treatment at a Colorado VA clinic. The email said that the OIG or an impartial VA official would review the issues she reported, which she said included whether the facility adequately addressed his access to a firearm.

Connor Brumfield, who grew up with a love for the military before joining the Army, crashed his car in November 2020 while still active duty, which caused a TBI and persistent problems with sleep, said his father, Brian Brumfield. He reported depression symptoms to the military after the crash, his father said.
Attending college in Montana after leaving the military, Connor Brumfield was “living his dream life” prior to being prescribed bupropion for depression in March 2023. He denied suicidality on a self-assessment completed the day he was prescribed bupropion by a Montana clinic.
Connor Brumfield died by suicide eight days after receiving the bupropion.
“This phenomenon is stripping our country of some of the best people we have,” Brian Brumfield said of the suicide deaths of young veterans.
Brian Brumfield filed a complaint about the prescription to the OIG in November 2024, though he said the office of his Congressional representative, Jim Jordan, told him the OIG did not find cause for investigation. The CW’s efforts to reach Jordan’s office were unsuccessful. A spokesperson for the OIG said the office could not discuss details about Brian Brumfield’s complaint due to privacy laws.
A spokesperson for the VA Eastern Colorado Health Care System, which includes the clinic Tyler Everett visited, did not provide comment in time for publication. Citing federal privacy laws, a privacy officer for the Montana VA Health Care System said the system could not legally comment on Connor Brumfield’s treatment.
Lack of informed consent and close monitoring
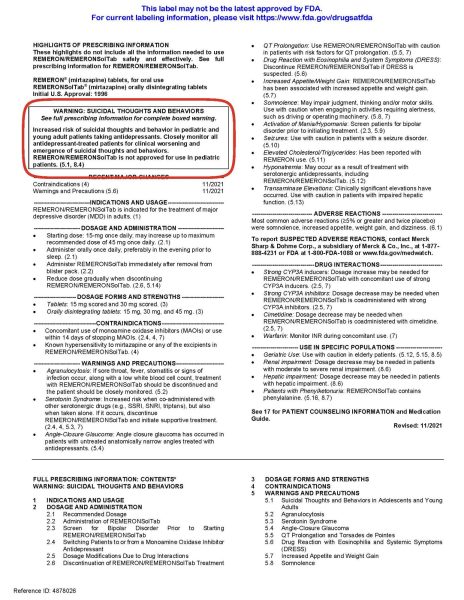
Connor Brumfield and Hunter Whitley were both prescribed antidepressants for which the FDA had issued black box warnings on the medication labels, cautioning about increased risk of suicidality for patients under 25 during the first few months of treatment.
Whitley’s OIG report said that the nurse practitioner violated VHA policy by not getting proper informed consent by discussing the warning with him before prescribing Remeron during his intake appointment.
The nurse practitioner also did not closely monitor him like the box warnings advised and should have planned for a provider to see him sooner than the two month follow-up appointment date the nurse had planned for, the report concluded.
To veterans advocate Derek Blumke, the VA’s “reckless” prescribing of psychotropic medications is causing part of the veteran suicide crisis. He said veterans are not receiving proper education as to the risks and efficacy of medications like antidepressants and that such medications are overprescribed.
Blumke was founding director of the VA VITAL program, which helped establish clinics on college campuses, including the one at the University. Blumke also served as a founding committee member for the National Action Alliance for Suicide Prevention, a public-private partnership, and he co-founded the Student Veterans for America.
According to the Grunt Style Foundation, a veterans advocacy organization, 28% of all veterans who had recently used VA care in 2019 were prescribed antidepressants, and 68% were on some type of psychiatric drug.
Experts said that high prescription rates of antidepressants are not necessarily evidence that they are overprescribed, and they are FDA approved to treat a variety of conditions. According to the CDC, depression is also a risk factor for suicide.
“Moral of the story here is they’re just not doing this safely nor smart,” Blumke said.
Moving forward
Hunter Whitley, Tyler Everett and Connor Brumfield also had another thing in common: Though their parents knew some — but not all — details about their mental health, the men’s deaths came as a shock.
“They say it’s always the person that you don’t expect, you know, and you would have never thought Hunter would die by suicide,” said Suzanne Hinton, Whitley’s aunt. “You would never have thought that.”
A recent Alabama Senate bill has been proposed to combat veteran suicide.
The Houston/Hunter Act — named in part after Whitley and another Alabama veteran who died by suicide, Houston Tumlin — aims to address high-risk veterans’ access to firearms by creating a legal framework for them to store guns temporarily in safe storage facilities.
Jason Smith — Alabama National Guard resilience and risk reduction coordinator and suicide prevention program manager, and an advocate for the bill — is spearheading the SAFER Together initiative to create a network of safe storage locations. Smith said the initiative’s implementation depends on the bill’s passage.
SAFER Together and the Houston/Hunter Act, he added, are part of a broader effort to combat stigma about mental health, as service members have lost more friends to suicide than they ever did in combat.
“In combat, we know who that enemy is,” he said. “When it comes to mental health and suicide prevention, it’s like the enemy is a stigma. You got to remove that, because that’s the number one enemy.”
Groups like the Student Veterans Association are also working to combat that stigma. Each year, the organization partners with the Auburn SVA to host Operation Iron Ruck, a 151-mile walk between Tuscaloosa and Auburn the week of the Iron Bowl, for veteran suicide awareness.
“When it’s 2 a.m. and you’re walking down that road, man, anything is open to talk about,” said Jordan Golden, advisor to the president of SVA and former president himself.
In December 2023, Whitley’s family established a nonprofit organization in his name: the Hunter Whitley Butterfly Initiative. The group works to break stigmas by promoting awareness and support for veterans mental health, through events like retreats for veterans, roundtable discussions and a yearly “Chasing Freedom 5k.”
The initiative’s name and logo come from an index card with a drawing of a butterfly that was found in Whitley’s room after his death. That drawing now sits framed in McDaniel’s living room.

Before the OIG report, as McDaniel said, butterflies initially represented the difficult transition to civilian life. But now, they also represent transformation.
“I think it’s time that we have some transformation within the VA healthcare system,” she said.